
L’influenza rimane una delle infezioni più ostinate e spiacevoli del pianeta.
Ritorna ogni inverno, mutando, eludendo il sistema immunitario e diventando infine resistente ai farmaci. Ora, gli scienziati stanno proponendo un approccio inaspettato che potrebbe letteralmente disattivare il virus a livello del suo codice genetico.
Si chiama SRISPR, ed è una tecnologia di editing genetico tipicamente associata al trattamento di malattie ereditarie rare, come strumento . Al Pandemic Research Alliance Symposium di ottobre, il virologo Wei Zhao del Peter Doherty Institute di Melbourne ha descritto un progetto che il suo team sta sviluppando con i colleghi.
L’idea è di utilizzare Crispr non per modificare il DNA umano, ma per colpire l’RNA del virus influenzale. Questo è importante perché il genoma dell’influenza è composto da RNA, il che significa che il virus ha un punto vulnerabile che può essere preso di mira. Quando si parla di Crispr, l’enzima Cas9, che agisce sul DNA, è solitamente menzionato più spesso. Ma in questa storia, Cas13, un parente meno noto di Cas9, gioca un ruolo chiave. Cas13 è in grado di tagliare l’RNA.
In natura, nessuno di questi enzimi è prodotto dalle cellule umane. Appartengono invece all’arsenale di batteri e archea, dove svolgono un ruolo nella loro difesa contro i virus. Gli scienziati vogliono trasferire temporaneamente questo principio alle cellule umane e costringerle a produrre brevemente Cas13, in modo che disattivi il virus dell’influenza.
Il formato di trattamento proposto sembra piuttosto pratico. Potrebbe trattarsi di uno spray nasale o di un’iniezione che fornisce istruzioni molecolari alle cellule del tratto respiratorio tramite nanoparticelle lipidiche. Il sistema è costituito da due parti. La prima è l’mRNA, che istruisce la cellula a produrre Cas13. La seconda è l’RNA guida, una sorta di indirizzo che indica a Cas13 esattamente quale parte dell’RNA virale tagliare. Secondo il team guidato dall’infettivologa Sharon Lewin, dopo questo intervento, il virus perde la capacità di replicarsi normalmente e l’infezione viene bloccata al suo livello più elementare.
Gli autori del progetto considerano la tecnologia non solo come un trattamento per l’influenza già in corso, ma anche come una potenziale misura preventiva. Ad esempio, durante le stagioni influenzali particolarmente gravi, le cellule respiratorie potrebbero essere preparate in anticipo alla difesa, consentendo loro di rispondere più rapidamente all’infezione. Il paragone di Zhao è semplice e chiaro. È come tenere i soldati armati prima ancora di incontrare il nemico.
Il principale vantaggio di questo approccio è che Cas13 può essere indirizzato alle cosiddette regioni conservate del genoma influenzale. Si tratta di frammenti di RNA presenti nella maggior parte dei ceppi e vitali per il virus. L’individuazione di queste regioni offre la possibilità di creare un farmaco ad ampio spettro efficace contro più varianti influenzali, anziché solo contro alcune varianti specifiche. Rispetto ai farmaci antivirali convenzionali, che perdono efficacia nel tempo a causa della resistenza, questa versatilità è particolarmente interessante.
Crispr-Cas13 non è l’unico candidato nella categoria dei cosiddetti farmaci pan-influenzali. Sono in fase di sviluppo anche anticorpi monoclonali, che mirano a colpire specificamente gli elementi resistenti del virus, così come farmaci che aumentano la produzione di interferoni, le molecole di allarme che scatenano l’attacco immunitario. Ma l’influenza è così ben adattata alla sopravvivenza che nessuno dei due approcci sembra una vittoria facile.
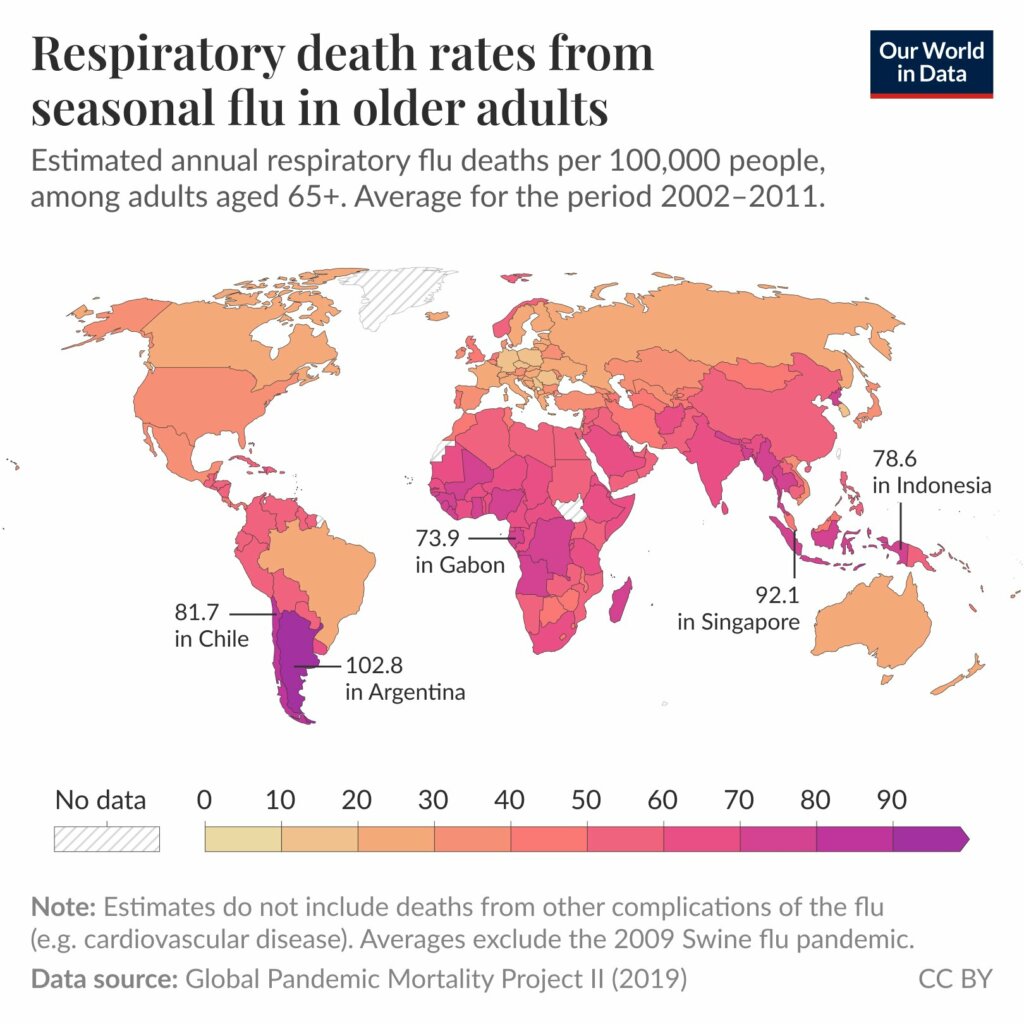
La motivazione a cercare nuove soluzioni è comprensibile. Si stima che la sola influenza A uccida tra le 12.000 e le 52.000 persone all’anno negli Stati Uniti, e la cifra varia notevolmente a seconda della gravità della stagione. In questo contesto, anche un’idea apparentemente audace diventa rapidamente oggetto di un acceso dibattito.
C’è anche scetticismo, ed è piuttosto pratico. Nicholas Heaton, professore di genetica molecolare e microbiologia alla Duke University, evidenzia due rischi. In primo luogo, Cas13 è una proteina estranea di origine batterica e l’organismo potrebbe innescare una risposta immunitaria contro di essa. In secondo luogo, permane il rischio dei cosiddetti effetti off-target, quando lo strumento colpisce non solo l’RNA virale, ma anche l’RNA della persona stessa.
Sono già stati effettuati i primi tentativi di valutarne la sicurezza. Il Wyss Institute dell’Università di Harvard sta utilizzando un modello “lung-on-a-chip”, in cui tessuto polmonare umano e cellule vascolari vengono assemblati in un microsistema che imita i processi del mondo reale. Questo è particolarmente utile per l’influenza grave, poiché durante tali infezioni il virus penetra in profondità negli alveoli, le minuscole sacche d’aria dove si replica attivamente. Secondo Donald Ingber, uno dei direttori dell’istituto e autore di questi modelli, gli esperimenti hanno dimostrato che le cellule addestrate a lavorare con Cas13 potrebbero sopprimere la replicazione di vari ceppi, tra cui H1N1 e H3N2. Il team non ha inoltre osservato effetti indesiderati off-target e, insieme all’attività virale, si sono ridotti anche i segnali infiammatori , che tipicamente aumentano durante l’infezione.
Nonostante risultati così incoraggianti, rimane un interrogativo, che non riguarda tanto il concetto in sé quanto la sua attuazione. Ingber sottolinea che indirizzare nanoparticelle lipidiche con istruzioni per raggiungere gli alveoli polmonari profondi è molto difficile. E Heaton sottolinea un’altra sfortunata caratteristica della natura. Anche se l’attacco colpisce regioni critiche del genoma, il virus può tentare di eludere la pressione mutando. Come afferma lui, “la natura di solito trova sempre un modo”, e queste storie spesso finiscono con l’agente patogeno che escogita una soluzione alternativa.
È interessante notare che Heaton sta valutando anche un’altra strategia, sempre correlata a Crispr, ma questa volta difensiva. Invece di attaccare il virus, potrebbero alterare l’ambiente corporeo per rendere più difficile al virus influenzale l’ingresso nelle cellule e la replicazione. Questa versione utilizza Cas9 , che aiuta a identificare i geni umani fondamentali per il ciclo vitale del virus. Gli scienziati stanno prendendo cellule umane, eliminando i geni uno a uno e testando se il virus influenzale mantiene la sua capacità di infettarle e ucciderle. Di conseguenza, hanno già identificato un bersaglio importante. Gli esperimenti dimostrano che il virus è altamente dipendente dal gene SLC35A1, responsabile della presenza di alcuni zuccheri sulla superficie cellulare. Questi zuccheri sono ciò che il virus influenzale utilizza come recettore, o punto di ingresso.
Sembra quasi un perfetto “interruttore di emergenza per l’influenza”, ma ha i suoi limiti.
Crispr-Cas13 promette di colpire direttamente l’RNA dei virus influenzali, tagliandolo e impedendo loro di replicarsi. Questo approccio rappresenta una svolta rispetto ai farmaci antivirali tradizionali, perché agisce a livello genetico, mirando alle regioni più critiche del virus. Tuttavia, identificare con precisione le sequenze da bersagliare è complesso, soprattutto considerando la rapidissima capacità dei virus di mutare.
L’intelligenza artificiale e i supercomputer entrano in gioco come strumento fondamentale per guidare Crispr in modo sicuro ed efficace. Algoritmi avanzati analizzano milioni di sequenze virali in tutto il mondo e prevedono quali regioni siano più conservate e vulnerabili. In questo modo, l’IA suggerisce le sequenze guida RNA ottimali per Cas13, riducendo il rischio di effetti indesiderati sulle cellule umane.
Oltre alla progettazione delle molecole, l’IA viene utilizzata per simulare l’interazione tra Cas13 e le cellule, anticipando possibili effetti off-target. Questo permette agli scienziati di ottimizzare sia le nanoparticelle che trasportano gli enzimi sia il dosaggio del trattamento, riducendo i rischi e accelerando la fase sperimentale.
Infine, l’intelligenza artificiale aiuta a prevedere l’evoluzione del virus e le possibili mutazioni che potrebbero renderlo resistente. Grazie a queste simulazioni, Crispr-Cas13 può essere progettato come una terapia adattiva, pronta a colpire non solo le varianti attuali, ma anche quelle future, aprendo la strada a una nuova generazione di antivirali “intelligenti”.
Né lo spray nasale a base di Crispr-Cas13 né le iniezioni sono ancora pronti per l’uso clinico. Ma l’idea stessa che l’influenza possa essere fermata non solo attraverso i sintomi e non solo attraverso il sistema immunitario, ma interferendo direttamente con il suo RNA, sembra un passo avanti verso una nuova classe di tecnologie antivirali. Se gli scienziati riusciranno a risolvere i problemi di somministrazione e sicurezza, l’influenza, che ha tenuto l’umanità con il fiato sospeso per decenni, potrebbe per la prima volta affrontare un avversario in grado di bloccarla a livello di codice.
Ti è piaciuto questo articolo? Ne stiamo discutendo nella nostra Community su LinkedIn, Facebook e Instagram. Seguici anche su Google News, per ricevere aggiornamenti quotidiani sulla sicurezza informatica o Scrivici se desideri segnalarci notizie, approfondimenti o contributi da pubblicare.

 Cybercrime
CybercrimeLe autorità tedesche hanno recentemente lanciato un avviso riguardante una sofisticata campagna di phishing che prende di mira gli utenti di Signal in Germania e nel resto d’Europa. L’attacco si concentra su profili specifici, tra…
 Innovazione
InnovazioneL’evoluzione dell’Intelligenza Artificiale ha superato una nuova, inquietante frontiera. Se fino a ieri parlavamo di algoritmi confinati dietro uno schermo, oggi ci troviamo di fronte al concetto di “Meatspace Layer”: un’infrastruttura dove le macchine non…
 Cybercrime
CybercrimeNegli ultimi anni, la sicurezza delle reti ha affrontato minacce sempre più sofisticate, capaci di aggirare le difese tradizionali e di penetrare negli strati più profondi delle infrastrutture. Un’analisi recente ha portato alla luce uno…
 Vulnerabilità
VulnerabilitàNegli ultimi tempi, la piattaforma di automazione n8n sta affrontando una serie crescente di bug di sicurezza. n8n è una piattaforma di automazione che trasforma task complessi in operazioni semplici e veloci. Con pochi click…
 Innovazione
InnovazioneArticolo scritto con la collaborazione di Giovanni Pollola. Per anni, “IA a bordo dei satelliti” serviva soprattutto a “ripulire” i dati: meno rumore nelle immagini e nei dati acquisiti attraverso i vari payload multisensoriali, meno…